What is osteoporosis?
Osteoporosis is a bone disorder where bones become thinner, lose their strength, and have a higher risk of breaking or fracturing. Bones in this state can fracture even during everyday movements such as coughing, bending or falling over, with the most common osteoporotic fractures occurring in the wrist, hip and spine.
Risk Factors
There are higher risks of osteoporosis development in women over the age of 50 (post menopause), or in populations with poor diets that are low in calcium, or where there is poor calcium absorption due to intestinal problems (eg. coeliac disease), in those with an overactive thyroid, a sedentary lifestyle with little to no weight baring exercise, use of medications such as prednisone, smokers, over-use of alcohol, or a family history of osteoporosis.
How is it diagnosed?
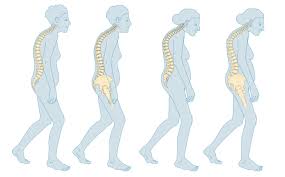
An early sign of osteoporosis can be a loss of height, caused by a curvature or compression of the spine, caused by a weakened vertebra, which develop tiny breaks called compression fractures. This can cause back pain or aching, but the loss of height alone usually does not cause any symptoms.
Bone density testing is really the only way to properly confirm that there is bone loss or less than ideal density. This is usually done with x-ray style scanning (DEXA Scan). Blood testing cannot provide an osteoporosis diagnosis.
What’s vitamin D got to do with it?
Vitamin D is an essential nutrient in the formation of healthy bone tissue due to its role in maintaining normal levels of calcium and phosphorus in the blood. Vitamin D increases the absorption of both phosphorus and calcium from food, and also plays a role in reabsorption of calcium back from the urine, forming in the kidney tubules.
When vitamin D levels or other bone formation minerals are low or insufficient, the body will reduce the update of phosphorus and calcium, or excrete it, as it cannot be utilised without the other nutrients. This includes deficiencies of magnesium, boron, and vitamin K2, as well as vitamin D. This can lead to poor bone density, and slow bone tissue repair from injuries.
It is this relationship with the other bone formation nutrients, that makes vitamin D so critical in the development of osteoporosis, and yet, more often than not, this nutrient is not tested in routine blood testing, even if osteoporosis has been identified or is suspected.
Should I take calcium supplements?
Calcium is in such a wide range of foods, the likelihood of a calcium deficiency in the western world is unlikely. Blood testing provides little information on status, as the body will always try to maintain a balance of blood calcium levels and will dissolve bone to increase levels if necessary, to keep levels constant.
Excessive vitamin D dosing, such as the mega doses often given by the medical system, can also lead to excessive calcium in the blood (hypercalcemia), and this can cause even more serious health problems. Only 1% of the body’s calcium is in the blood stream, and is involved in nerve excitability and conduction, cardiac and skeletal muscle function, cell membrane permeability and cellular adhesiveness. The body works very hard to keep levels just right, and mega dosing of vitamin D can cause major disharmony to this balance, as can the mega dosing of calcium.
Excess calcium will cause the body to excrete it via the kidneys. It does not create bone tissue in the absence of vitamin D, magnesium, boron and vitamin K2. Calcium deposits can harden the delicate kidney tubules or other arteries and blood vessels, a problem that is difficult to reverse. Calcium deposition can occur in many areas of the body including; brain basal ganglia (causing brain and cognitive problems), cornea and conjunctiva (causing issues with eyesight), heart muscle and arterial linings (causing blood pressure dysfunction), lungs, pancreas, soft tissue around the joints (causing joint pain and arthritis), eardrum and middle ear bones (causing hearing impairments). This type of calcification occurs whenever calcium levels, vitamin D or phosphate levels become too high for a long enough period.
Calcium is prevalent in so many foods, only the poorest of diets would result in a deficiency. While dairy foods are well known for their calcium content, there are many other foods that contain even more amounts or come in forms that are better absorbed in the digestive system. These include nuts and seeds, yoghurt, cheese, small fish with eatable bones (sardines, canned salmon, anchovies), beans, lentils and all legumes, leafy greens, rhubarb, tofu and other soy based products and figs.
While these foods are high in calcium, almost all plant-based foods, meats and seafood contain some levels of calcium, so anyone who adopts a whole food lifestyle, would most certainly be consuming more than enough. Where most people struggle nutritionally, is with other nutrients such as vitamin D and magnesium, which are often found to be deficient.
What about post menopause?
Oestrogen slows down the breakdown of bone, and the loss of oestrogen during menopause, can lead to an increased risk of poor bone health. Some women have decided to use hormone replacement therapy, however, this comes with several high risks such as an increased risk of heart disease, stroke or breast cancer, making it a less than desirable solution.
Often post-menopausal women will be low in nutrients such as magnesium and vitamin D, and simply correcting these deficiencies greatly reduce the risk of bone loss.
An overactive thyroid can also cause bone loss, and those who take thyroid medications should have their levels checked regularly, to ensure their medication is not too high, or look for more natural ways to rebalance their thyroid function.
Why is Digestive Health Important?
A happy and healthy digestive system is the pinnacle of optimal health. The strength of the immune system, nutrient absorption, elimination of toxins and the availability of vitamin D are all reliant on a healthy digestive system that is free from inflammation and has a balanced microflora. The western diet is so full of processed and inflammatory foods, it is no wonder that vitamin D deficiency is so prevalent.
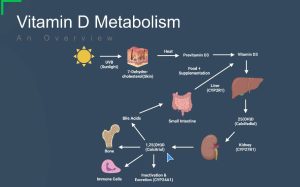
The health of the liver is also paramount in achieving optimal health, as it is here, that the pre-vitamin D3, created by the sun hitting the skin, and converting LDL cholesterol, allows the conversion of the D3 to calcifediol, which is then sent to the kidneys for further conversion and distribution to the immune system, muscles, bones and to the digestive system to create bile acids. Any impairment in this process, could see good levels of D3, yet poor bone or immune system health, as the D3 is not converting to a form that can be utilised by these systems.
So how can we Prevent Osteoporosis or minimise the risks?
There are many natural ways that we can reduce the risk of developing osteoporosis as we age, without the need for pharmaceutical intervention. These include;
- Daily Exercise, including some weight baring exercise several times per week
- Optimal vitamin D levels (over >100nmol/L)
- Optimal digestive function with a healthy microbiome and nutrient absorption
- Whole food diet, that includes a variety of 80% vegetables, 20% animal protein
- Include food sources of vitamin D (fatty fish like salmon, eggs, chicken liver)
- Safe daily sun exposure with exposed skin
- Avoid smoking and excessive alcohol consumption
